Fractured Neck of Femur (FNOF)
Hip fractures are a common occurrence worldwide, with both a significant impact on the affected individuals as well as the healthcare system. The consequences of hip fractures can be severe, leading to decreased mobility, increased risk of complications, and a lower quality of life.1-3
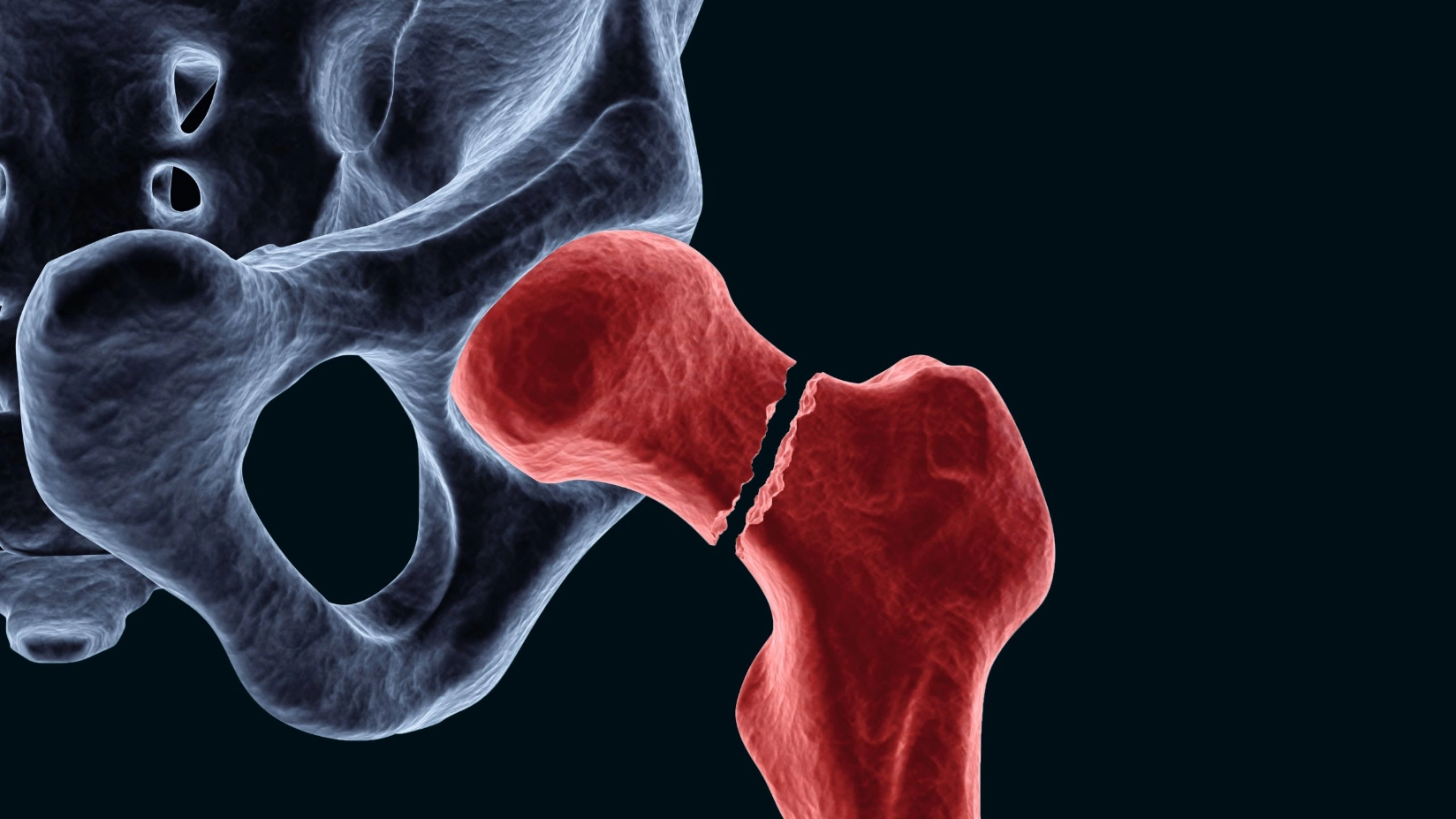
Hip fractures, particularly fractured neck of femur (FNOF), affect individuals of all age groups, however they are more common in the elderly population. This is generally due to low-energy falls and is therefore often associated with osteoporosis.1,4 Proximal femur fractures generally require hospitalisation and surgical treatment, frequently leading to disability and being associated with high morbidity and mortality.1,3,5
The treatment of FNOF with a hemiarthroplasty is considered an option for less fit and less mobile patients with lower life expectancy. Advantages of hemiarthroplasty include a short operation time and quick mobilisation of the patient associated with acceptable clinical, functional, and radiological outcomes.6
Cemented Hemiarthroplasty after FNOF
Hemiarthroplasty can be performed using either cemented or uncemented prostheses. Cemented hemiarthroplasty involves the use of bone cement to secure the prosthesis and has been shown to offer several advantages over uncemented hemiarthroplasty. It is associated with fewer complications, including less intraoperative and periprosthetic fractures, as well as a lower amount of dislocations or infections, thus leading to a reduced risk of revision compared to uncemented hemiarthroplasty.7-9
Furthermore, patients undergoing cemented hemiarthroplasty experience better mobility within the first year of surgery, along with a modest but significant improvement in quality of life.9,10
As a result, national guidelines for hip fracture management recommend the use of cemented stems with this approach.11,12
Dual Antibiotic-Loaded Bone Cement Reduces Risk for Infection in Hemiarthroplasty after FNOF13-16
Periprosthetic joint infection (PJI) remains one of the most prevalent complications among FNOF in hemiarthroplasty. The occurrence of PJI in FNOF patients is much more frequent and even more devastating than in patients undergoing elective hip replacement.17
The use of antibiotic-loaded bone cement (ALBC) covers one significant aspect of local infection prevention among others.
A meta-analysis from 2024 found that using high-dose dual ALBC (DALBC) may offer a better infection prophylaxis in hip surgeries than low-dose single ALBC (SALBC). Among the hip fracture data, five studies with a total of 8,985 FNOF patients were included in the meta-analysis.18
Across four studies, the use of DALBC reduced the risk for infection to similar levels ranging between 1.1-1.2 %.13-16
Thus, the use of a DALBC such as COPAL® G+C can effectively lower the risk of PJI and its sequelae in higher risk patients.
| Sprowson et al. 2016 | Tyas et al. 2018 | Savage et al. 2019 | Agni et al. 2023 |
|---|---|---|---|
| n = 848 | n = 1.941 | n = 206* | n = 4.936 |
| 12 months Follow-up | n.a. | 12 months Follow-up | 90 days Follow-up |
* including 26 total hip arthroplasty cases